Concussion Assessment & Management
A look at treatment options and rationale for application
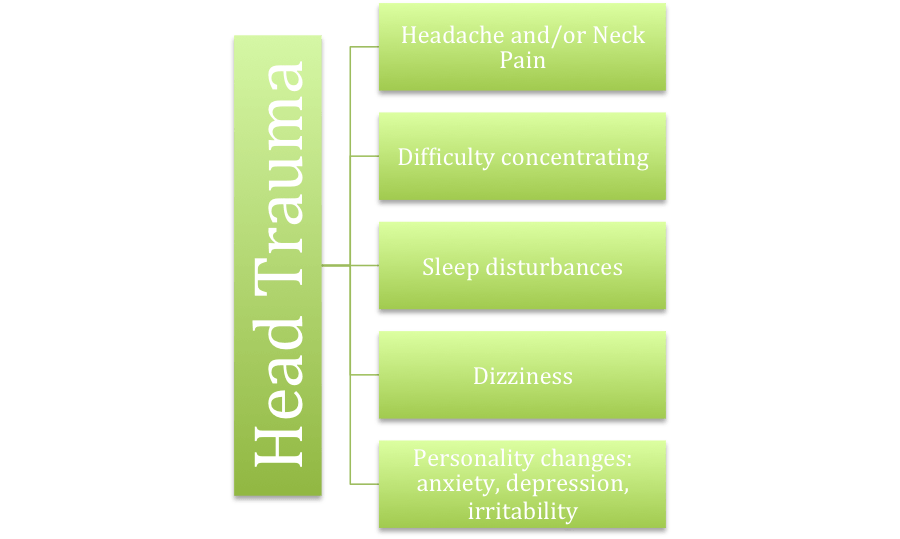
Sports concussion management has become a hot-topic recently as athletes have become faster and stronger equating to higher impact collisions with opponents, playing fields, equipment and teammates. Youth are getting involved in organized sports at younger ages putting a greater number of children at-risk for injury. Large amounts of money, notably driven by the NFL and NCAA, have poured into research in order to identify risk factors, indicators of recovery, effective rehab programs and prevention measures with respect to concussions. Concussions often occur in sports arenas; however they are also a concern following head trauma as the result of falls, blast-type injuries from military service, motor vehicle accidents or even non-contact whiplash injuries. Each of these scenarios can include similar presentation of symptoms, but some characteristics are often unique to the trauma involved. Along with physical trauma to the brain which can create further vascular and chemical effects that perpetuate prolonged effects, other systems can also be involved which can contribute to the clinical picture. Commonly reported symptoms are headache, dizziness, difficulty sleeping, imbalance and irritability.
These symptoms are often reported in issues involving the cervical spine (cervicogenic) as well as the vestibular system – without head trauma . Therefore it is essential for healthcare providers to determine the system and pathology that is causing prolonged symptoms. Researchers agree that most symptoms resolve in 7-10 days, however in 10-15% of the cases, individuals notice symptoms persisting weeks to months. [1] There are also factors suggesting who may be more vulnerable to persistent symptoms such as younger populations, females, and those with a pre-existing cognitive disorders (ADHD) or affective disorders (depression, anxiety). [2] It is important to determine in these cases if the pathophysiology of concussion is still at fault for symptoms or an independent system such as the neck (cervical) or inner ear (vestibular) or visual system.
The overlapping nature of the cluster of symptoms makes it important to clinically test each system’s influence on the patient’s presentation in order to fully address any impairment. For example, rest may be the best treatment of the physical and chemical trauma to the brain however prolonged rest (>2-3 days) may only exacerbate cervicogenic, physiologic or vestibular dysfunctions. This makes for protracted symptoms and potentially worsening symptoms if an athlete attempts to return to their sport.
Consensus on best practices for the management of concussion patients is marginal – guidelines are presented and revised, different groups have specific parameters for measuring progress through phases and benchmarks for return to sport. Guidelines and protocols are likely difficult to nail down due to the individual nature of the type of injuries, pre-injury status of all the systems involved and effects of treatment strategies on the various structures involved in a rehab program. The important components of a rehab program need to address the cognitive, vestibular, physical and psychological dysfunctions that can be present in individuals who have suffered concussions.
The American Physical Therapy Association (APTA) has a recommendation for the evaluation and management of concussions based on the most recent evidence which includes:
1. Rest from both cognitive and physical exertion – evidence is supporting that prolonged rest is not necessarily better than progressive return to activities [3]. Knowing when to begin and how intense activity should be is an essential element to the plan of care.
2. Protection from additional injury . There is increased vulnerability for repeat concussion while the brain is healing from a current concussion (Second Impact Syndrome). Second Impact Syndrome is rare, but catastrophic. It occurs only in young people (<23 years) and has a mortality rate of 50% when it occurs.
3. Neurocognitive assessment helps determine recovery stage, which is often performed by neuropsychologist, the individual’s school or allied health professional.
4. Balance Testing is helpful to establish presence of concussion and track of recovery
5. Physical therapy such as manual interventions and stabilization training for persistent neck pain and headaches when indicated; as well as threshold controlled strength and conditioning to improve physiologic homeostasis; vestibular and/or visual training for dizziness and imbalance
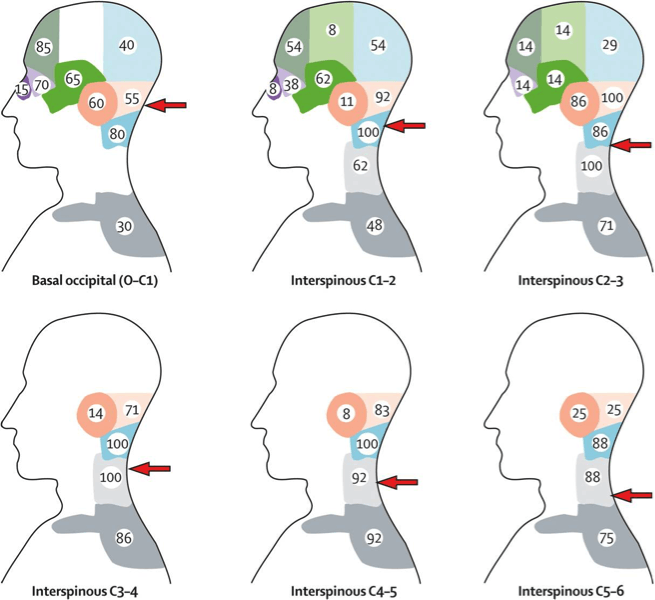
The APTA’s position and experience from the clinical evidence on physical therapy for concussions shows that up to 79% of patients report dizziness and 56% experience balance impairments following a sports concussion [4]. Post-concussive dizziness and headaches may arise from several sources including benign positional paroxysmal vertigo (BPPV), visual disturbances, post-traumatic migraines, labyrinthine concussion, neck dysfunction. Vestibular therapy has been shown to be effective in managing patients following concussion who continue to experience ongoing imbalance or dizziness without spontaneous resolution [5]. Specific interventions for cervical issues can also help to address headaches, neck & facial pain, dizziness and balance issues. A separate blog article touches on the pathology of a mild traumatic brain injury here. Evolution Sports has created a treatment and assessment algorithm to identify the full cause of unrelenting symptoms: physiologic (HR/BP), cervicogenic, vestibular, visual.
Pain referral patterns in upper cervical dysfunction
The physical therapists at Evolution Sports have specialty training in manual therapy, differential diagnosis as well as vestibular diagnosis and treatment in addition to having a special interest in return to sport training. They are all certified or working toward completion of certification in manual therapy. They have access to a team of neurologists, pediatric orthopedists and audiologists as referral resources if your care exceeds the scope of physical therapy or additional testing is necessary for progression of your plan of care. Your physical therapist at Evolution Sports is looking forward to developing a patient and symptom-specific rehab guideline for you or your loved one based on the most up to date research.
[1]McCrory P, et al. Consensus Statement on Concussion in Sport – 4th International Conference on Concussion in Sport held in Zurich Nov 2012 . Clin Sport Med. 2013 Mar; 23(2). 89-117.
[2]McCauley SR, Boake C, Levin HS, Contant CF, Song JX. Post-concussional Disorder Following mild to moderate TBI; Anxiety, Depression and Social Support as Risk Factors and Co-morbidities. J Clin Exp Neuropsychol. 2001 Dec; 23(6): 792-808.
[3]Leddy JJ, Kozlowski K, Donnelly JP, Pendergast DR, Epstein LH, Willer B. A preliminary study of subsymptom threshold exercise training for refractory post-concussion syndrome. Clin J Sport Med. 2010 Jan; 20(1):21-7.
[4]Lovell MR, Iverson GL, Collins MW, Podell K, Johnston KM, Pardini D, Pardini J, Norwig J, Maroon JC. Measurement of sypmtoms following sports-related concussion… Appl Neuropsychol. 2006; 13(3): 166-74.
[5] Alsalaheen BA 1, Mucha A , Morris LO , Whitney SL , Furman JM , Camiolo-Reddy CE , Collins MW , Lovell MR , Sparto PJ. Vestibular Rehabilitation for Dizziness and Balance Disorders after Concussion . J Neurol Phys Ther. 2010 Jun; 34(2):87-93.