Concussion By The Numbers
A look at the pathophysiology and incidence rates of concussion
Concussions, also known as traumatic brain injuries (TBI), have been a common topic in the news and medicine recently. The Centers for Disease Control and Prevention (CDC) recently rolled out new guidelines for the identification and management post-concussion. The CDC states that a TBI can range from mild (brief change in mental status or consciousness) to severe (an extended period of unconsciousness or memory loss after the injury. Mild forms of TBI are commonly called concussions [1]. We know that brain injuries can happen anywhere – from a fall in the yard to a motor vehicle accident – and they can happen at any age. However there are an increasing number of sports-related concussions and the greatest demographic affected by such head injuries are high schoolers. Some of the reasons for this are behavioral, environmental and physiological. Kids are entering structured sports at earlier ages giving them more potential "exposures" for injury. The brains of children are also still developing and injuries at younger ages will have longer potential effects.
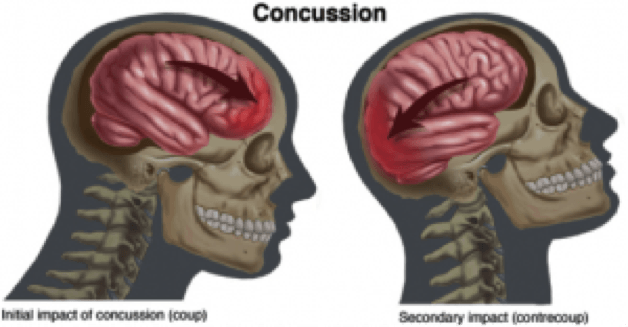
Head injuries will cause a double impact scenario: 1) head contacts object 2) object propels head in the reverse direction causing a second impact on the opposite side of the brain. However the idea of getting your “bell rung” belies the true issue and long term implications of a mild TBI.
It’s not simply deciding how bad the goose egg will be or icing down the inflammation from the hit. The impact of the head and the shearing of connections between the head and brain sets off a cascade of metabolic, physiological and microstructural injuries to the brain. The whiplash injury that can occur from the neck can cause headaches, dizziness and/or neck pain. Traumatic brain injury can affect the control center of our bodily functions not under conscious control, such as breathing, heartbeat and digestive processes. This system is called the autonomic nervous system (ANS). Concussions also can affect the control of both the cerebral brain flow (CBF) and cardiac rhythm. [2] Disrupting this chemical and metabolic system can cause potential concentration issues, dizziness and exercise-induced symptoms, among other complaints. The pathophysiology needs to be understood in order to best treat the wide-ranging presentation of symptoms.
With media attention turned toward long-term effects as well as untimely deaths related to head injuries, professional sports and the NCAA have invested large amounts of money into current research for assessment and treatment of concussions. As healthcare professionals we are now trying to utilize this information to best identify and treat patients.
Here are some numbers from the CDC on concussion overview…
- In 2013, about 2.8 million TBI-related ER visits, hospitalizations and deaths occurred in the US
- Over the span of six years (2007-2013), TBI-related ER visits increased by 47%
- In 2012, an estimated 329,290 children (age 19 or younger) were treated in US ERs for sports and recreation-related injuries that included a diagnosis of concussion or TBI
- From 2001 to 2012, the rate of ER visits for sports and recreation-related injuries with a diagnosis of concussion or TBI, alone or in combination with other injuries more than doubled among children.
The increased reporting is not surprising given the recent attention, but expect education from healthcare providers instead of a slew of medical testing at an initial medical appointment. Recent evidence has not supported routine imaging (x-rays, MRI) or blood tests to identify the presence or severity of a concussion. [3] For further potential treatment in the case of prolonged symptoms, see our separate blog here.
As stated earlier, concussions can happen anywhere to any person. The CDC reports that falls are the leading cause of head injuries reported to the ER for all but one age group: 15-24 year olds. Being struck by or against an object was the leading cause of TBI-related ER visits for this age group. In a study conducted by Meehan, et al in 2011 found that approximately 9% of all high school sports injuries are concussions – that’s almost 1 out of 10 injuries! [4]
Concussion Rates per Sport
The below numbers indicate the amount of sports concussions taking place per 1,000 athletic exposures. An athletic exposure is defined as one athlete participating in one organized collegiate athletic practice or competition, regardless of the amount of time played.
Injury Rate Per Exposure Based on Sport in Collegiate Athletes 1998-2004 [5]
| Women’s Ice Hockey |
0.91 |
| Men’s Football (American) |
0.54 |
| Men’s Ice Hockey |
0.41 |
| Women’s Soccer |
0.41 |
| Men’s Soccer |
0.28 |
| Men’s Lacrosse |
0.25 |
| Women’s Lacrosse |
0.25 |
| Women’s Basketball |
0.22 |
To learn more about Concussion Management , contact the Physical Therapists at Evolution Sports ! Early treatment is key to a successful outcome!
1. Centers for Disease Control and Prevention (CDC), National Center for Injury Prevention and Control. Report to Congress on mild traumatic brain injury in the US: steps to prevent a serious public health problem. Atlanta (GA): Centers for Disease Control and Prevention; 2003.
2. Leddy J, Baker JG, Haider MN, Hinds A. A Physiological Approach to Prolonged Recovery from Sports-Related Concussion . J Athl Train 2017 Mar; 52(3). 299-308.
3. Lumba-Brown A, Yeates KO, Sarmiento K. Diagnosis and Management of Mild Traumatic Brain Injury in Children . JAMA Pediatr. Published online Sep 4 2018. doi 10.1001
4. Meehan WP. Assessment and Management of Sports-Related Concussion. AM J Sports Med. 2011 Nov; 39(11): 2304-10.
5. Hootman J, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports … J Athl Train. 2007; 42(2): 311-319.