Can Physical Therapists Treat Temporomandibular Joint Dysfunction?
Of course! The TMJ is not unlike any other joint in the body, it contains a joint capsule, ligaments, and periarticular musculature. If it is not unlike any other joint, then why is it so intimidating to treat and why do such a small percentage of patients with jaw pain seek care?
Many Physical Therapists are intimidated to treat the TMJ due to the increased working knowledge of anatomy and biomechanics required to treat patients in this niche population, as well as the regional interdependence with the cervical and thoracic spine.
Chronic TMD
Chronic TMJ pain is cited to be the third most prevalent chronic pain condition worldwide, after tension headaches and low back pain. However, it is very underrepresented in physical therapy clinics, which I believe is in part due to the general population being unaware of how much a Physical Therapist can help with their condition.
Another variable that is associated with the chronicity of TMJ pain, is central sensitization. Central sensitization is defined as increased responsiveness of nociceptive neurons in the central nervous system to their normal or subthreshold afferent input. In other words, with chronic pain your brain may become sensitive to input and perceive this as pain during stimulation that was previously painless. Physical therapists are trained to decrease this sensitization with modalities and exercise, which will be discussed later
So what can a Physical Therapist do for Temporomandibular Joint Dysfunction (TMD)?
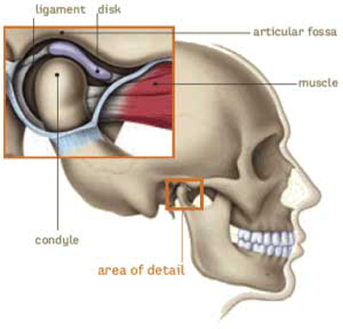
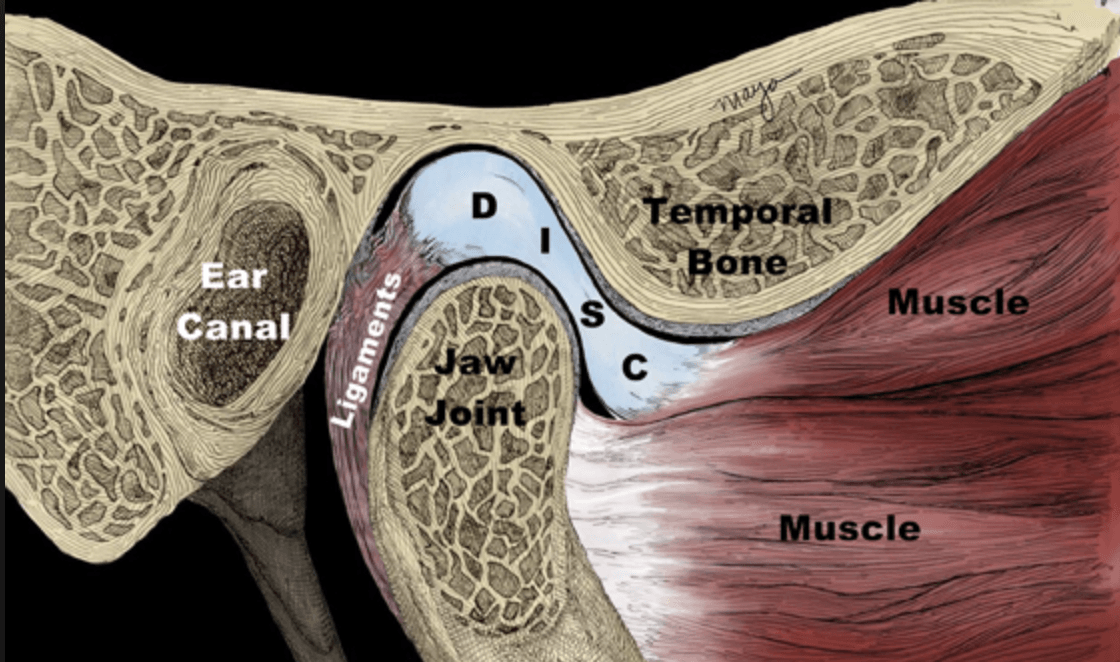
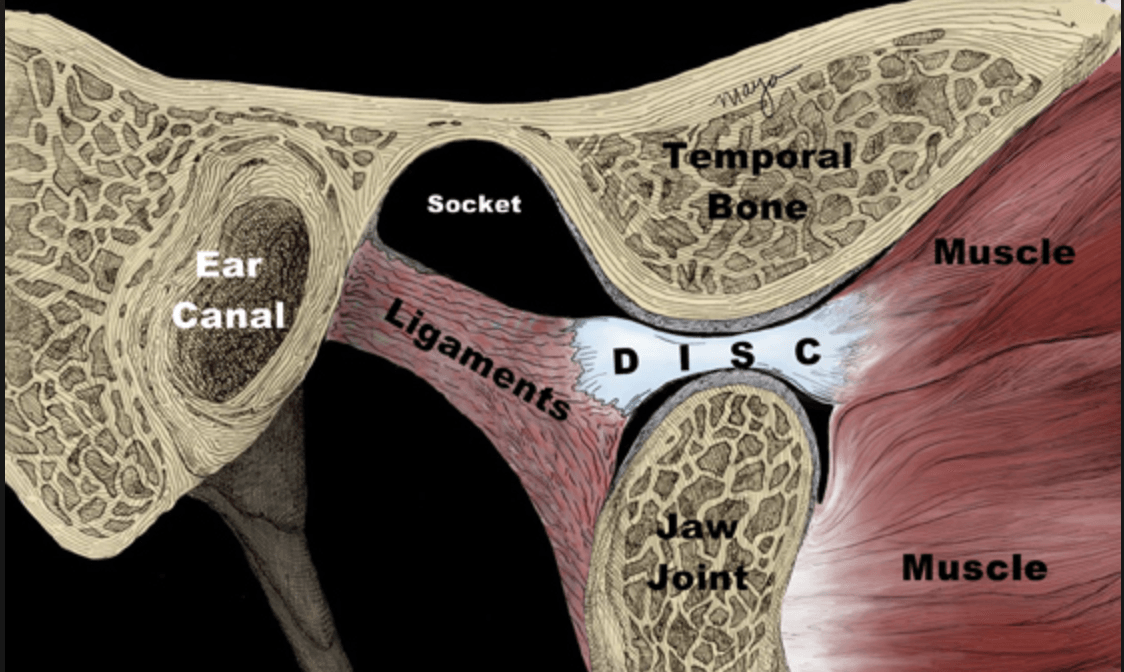
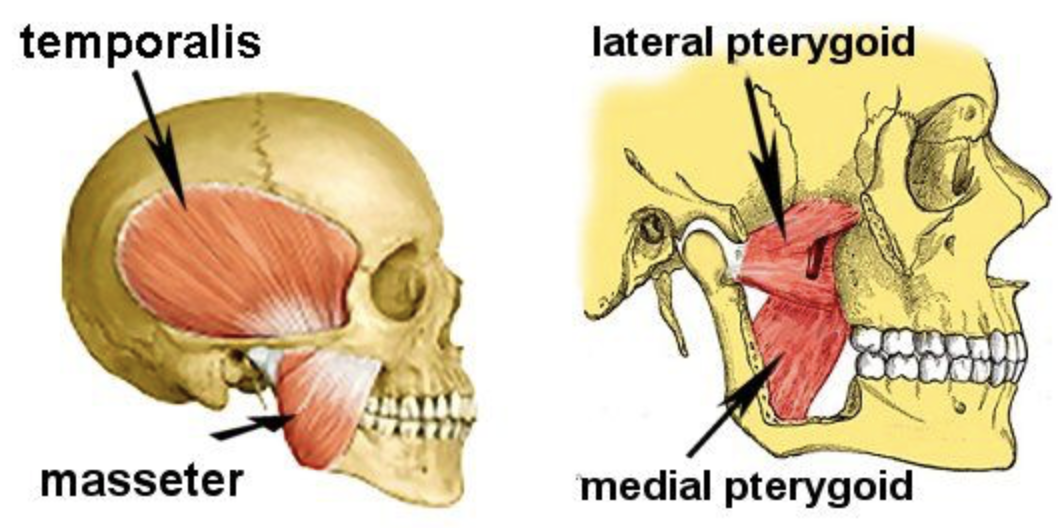
First, we must look at the anatomy of the joint:
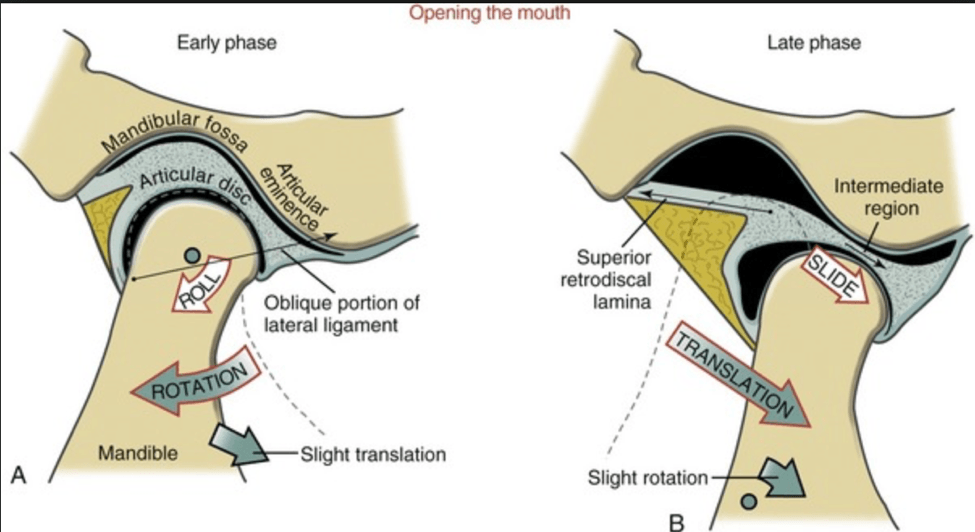
In the highlighted square, you will see the TMJ, with the bony components comprised of the condyle and the articular eminence. In between these bones you will see the articular disc, which serves to increase the congruency of the joint, similar to the menisci in the knee. However, the disc must move to maximize the available opening range of motion. In the pictures below, note how the disc moves forward when opening the mouth, and how the condyle remains under the disc.
Generally speaking, the initial goal of Physical Therapy (PT) will be to restore the normal biomechanics of the TMJ illustrated above, and identify which structures are preventing this from happening. The most common culprit of TMJ pathology, is the lateral pterygoid, which is the muscle pictured on the right side that attaches to the disc. If this muscle is tight or in spasm, it will pull the disc forward, which can lead to increased pain due the disc being pinched with opening and the lack of congruency of the joint in a resting position.
This is where the expertise of a skilled physical therapist is required. If a patient has tight quads or upper traps, it is relatively simple to perform soft tissue mobilization, stretching, or other modalities to address this tightness. However, it is less obvious how to address lateral pterygoid irritation.
While the lateral pterygoids play a large role in TMD, you will see below that there are several other muscles that assist in causing motion at the TMJ:
The temporalis and the masseter are much easier to locate, and you will be able to feel them contracting when clenching your jaw.
What does the research say about interventions to address TMD?
Soft tissue release/mobilization: Manual soft tissue techniques targeting the temporalis and masseter have been shown to effectively decrease pain (Gauer and Semidey, 2015). However, the ability to palpate and perform soft tissue mobilization to the lateral/medial pterygoids is much less reliable (Stelzenmueller et al 2016).
Bottom line: Manual soft tissue techniques have a positive effect on accessible muscles such as the temporalis and masseter, thereby improving symptoms associated with TMD, but they are unlikely to reach the pterygoid muscles that are not only more intimately related to the joint itself, but also more likely one of the primarily etiologic factors in TMD (Dunning et al 2017)
Dry Needling (DN): Due to difficulty palpating and mobilizing the pterygoids, increased focus has been placed on DN to address muscular irritation. As previously mentioned, the pterygoids are more likely to contribute to TMD, which increases the importance of addressing them with skilled physical therapy. Mesa-Jimez et al. performed DN 3x/week to the lateral pterygoids, and reported statistically significant within group improvement in pain and jaw range of motion, which was maintained at follow up 6 months after the intervention. A more recent study by Gonzalez-Perez et al. reported significant between group reductions in pain when comparing lateral pterygoid dry needling to methocarbamol (muscle relaxer).
Joint Mobilization: For any joint to achieve full range of motion, you also need appropriate movement of the bones on each other (arthrokinematics). While arthrokinematics are beyond the scope of this blog, understand that the condyle must first roll under the disc, and will then need to slide forward with the disc towards the articular eminence.
To determine if the TMJ is having difficulty rolling or sliding, your Physical Therapist will want to observe full opening, and will determine if the mouth opens straight down, or deviates to a certain side. If this is the case, joint mobilizations may be performed by a Physical Therapist to restore normal arthrokinematics. Martins et al. notes a general consensus in the literature that supports joint mobilization for improving pain and range of motion patients with TMD. They also reported a large effect and a significant difference in active mouth opening and pain reduction of manual therapy compared to other active interventions such as home exercise, massage, and splint therapy.
So now that I am out of pain, how do I prevent this from happening again?
As mentioned earlier, the initial phase of Physical Therapy is to decrease pain and restore motion for the TMJ, but how do we make sure this pain does not return? The mainstay of avoiding return of TMD is addressing postural deficits. If you are reading this, I want you to sit up nice and tall and open your mouth as wide as you can, now close and repeat opening while in a slumped forward posture. When slumped forward, the TMJ experiences increased stress on the capsule, as well as increased muscular demand to maintain the joint in appropriate position.
How can a Physical Therapist fix my posture?
Postural deficits are multifactorial in nature with some of the most common deficits being:
- Prolonged sitting
- Weak scapular stabilizers
- Weak cervical flexors
- Joint restrictions in thoracic or cervical spine
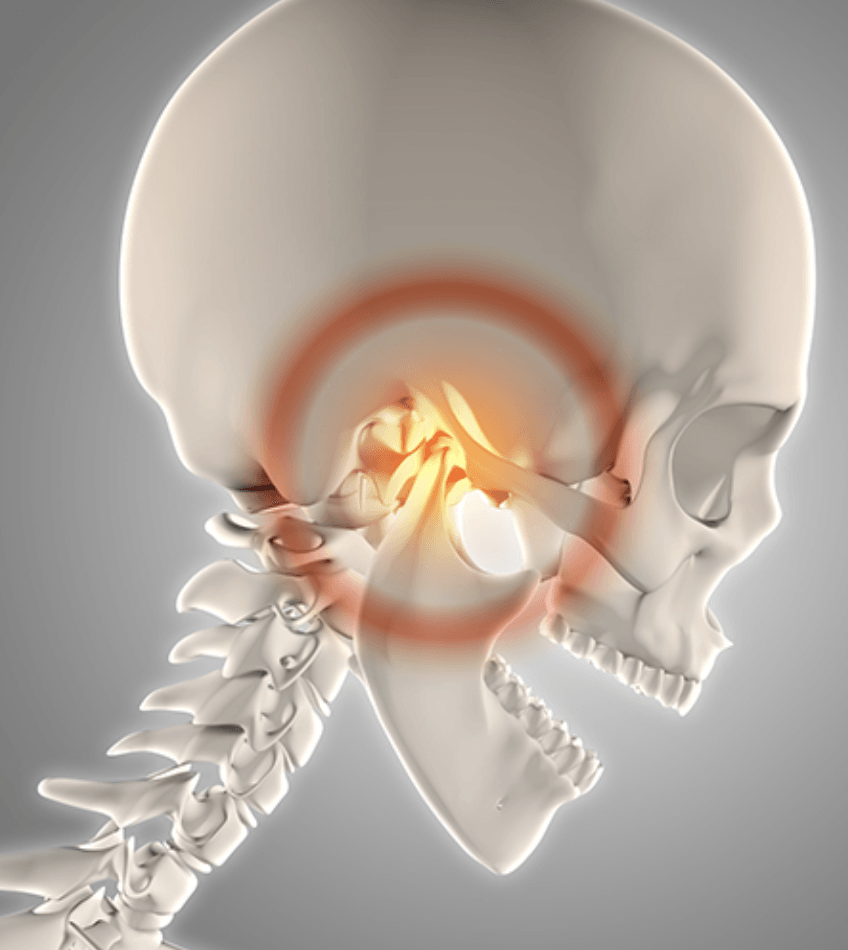
Regional interdependence:
Addressing the above deficits is essential to avoiding future TMJ issues, and should be started from day 1 in Physical Therapy. Looking at the picture above for reference, you can imagine that if the cervical/thoracic spine is not moving as much as it should, it will be difficult to maintain your head in the optimal position for the TMJ. This is why your Physical Therapist may recommend cervical and thoracic spinal manipulations, which is evidenced by numerous studies in a systematic review by Armijo-Olive et al. to have a statistically significant impact on TMD.
When this new range of motion is attained and the TMJ is in a good resting position, it is imperative to prescribe therapeutic exercises to maintain this position. Some examples of these exercises are chin tucks, mid trap rows, and cervical isometrics.
Cervicogenic headaches are also common to see with people suffering from chronic TMD. Cervicogenic headaches are defined as a chronic headache that arises from the upper cervical joints and/or musculature. They are believed to occur at the converging of the trigeminal and cervical afferents at the trigeminocervical nucleus within the upper cervical spinal cord. In other words, this converging of sensory fibers allows for the referral of pain signals from the upper cervical spine to areas of the face and head. This can be addressed by the use of upper cervical spine manipulation, as well as dry needling. For more information on cervicogenic headaches, see previous blog post written in November 2018.
Conclusion:
TMJ pathologies are multifactorial in nature, and are closely intertwined with adjacent areas. A Physical Therapy plan of care is not complete unless it addresses all of these factors, at the risk of symptoms returning. The Therapists at Evolution Sports Physiotherapy understand the complexity of the TMJ and how to treat it thoroughly..
Sources:
1. Butts, R. Dunning, J. Pavkovich, R. Metille, J. Mourad, F. Conservative management of temporomandibular dysfunction: A literature review with implications for clinical practice guidelines (Narrative review part 2). Journal of Bodywork & Movement Therapies 2017
2.Gauer, R.L., Semidey, M.J. Diagnosis and treatment of temporomandibular disorders. Am. Fam. Physician . 2015;91:378–386
3.Stelzenmueller, W., Umstadt, H., Weber, D., Goenner-Oezkan, V., Kopp, S., Lisson, J. Evidence - the intraoral palpability of the lateral pterygoid muscle - a prospective study. Ann. Anat. 2016;206:89–95
4.Dunning, J., Butts, R., Mourad, F., Young, I., Flannagan, S., Perreault, T. Dry needling: a literature review with implications for clinical practice guidelines. Phys. Ther. Rev. 2014;19:252–265
5.Dunning, J.R., Cleland, J.A., Waldrop, M.A., Arnot, C.F., Young, I.A., Turner, M., Sigurdsson, G. Upper cervical and upper thoracic thrust manipulation versus nonthrust mobilization in patients with mechanical neck pain: a multicenter randomized clinical trial. J. Orthop. Sports Phys. Ther. 2012;42:5–18
6.Gonzalez-Perez, L.M., Infante-Cossio, P., Granados-Nunez, M., Urresti-Lopez, F.J., Lopez-Martos, R., Ruiz-Canela-Mendez, P. Deep dry needling of trigger points located in the lateral pterygoid muscle: efficacy and safety of treatment for management of myofascial pain and temporomandibular dysfunction. Med. Oral Patol. Oral Cir. Bucal . 2015;20:e326–333
7.Armijo-Olivo, S., Pitance, L., Singh, V., Neto, F., Thie, N., Michelotti, A. Effectiveness of manual therapy and therapeutic exercise for temporomandibular disorders: systematic review and meta-analysis. Phys. Ther. 2016;96:9–25